This is the third part of our series about the condition based on our patient booklet “Fast Facts for Patients: Non-small Cell Lung Cancer with KRAS Mutation”. This article explains the role of genes, oncogenes, driver mutations and biomarkers in non-small cell lung cancer (NSCLC).
More about Genes and Cancer
Cancer treatment has been developing over the past few decades. Genes can become abnormal, enabling cancers to grow and spread; researchers are now finding ways to target these abnormal genes. To understand this type of treatment, which is often referred to as ‘targeted treatment’, it helps to understand a bit about how cancers start.
Everything that cells do starts with their genes, which are made of DNA and carry instructions for making proteins. Normal cells need these proteins to work properly. Proteins control how cells grow and become specialized, as well as controlling every function of each cell.
Gene Mutations and Cancer
Cells can become cancerous because they have changes (mutations) in their genes. Some mutations are inherited from a parent, are present from birth, and can be passed on to children. Others develop during a person’s lifetime and can’t be passed on.
Mutations cause the affected genes to make abnormal proteins that can prevent the cell from working properly. Not all mutations result in a cancer. But some give the cell properties that make it more likely to become cancerous if it collects a few more mutations.
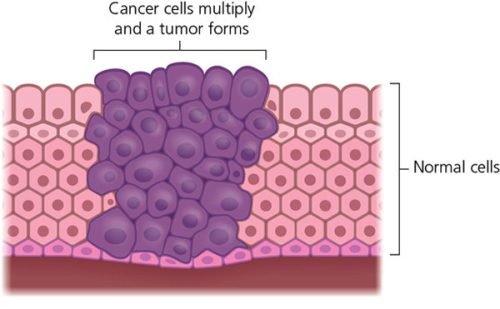
The most obvious cancer-causing mutations are those that cause the cell to keep multiplying when it shouldn’t. Normally in adults, most cells only reproduce to replace worn-out cells and repair damage. But cancer cells carry on multiplying much more quickly than normal cells do. The excess cells form a lump – a tumor.
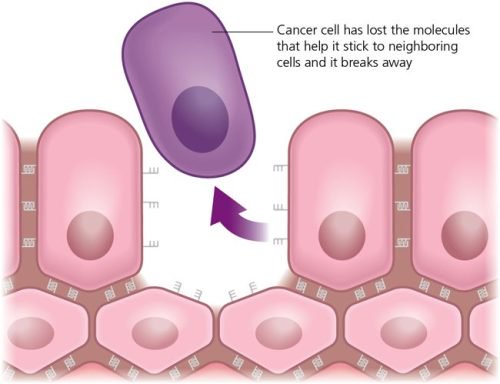
There are other mutations that mean the cells lose their ability to stick together. This is one reason why cancers are able to spread. Cancer cells can break away and travel through the blood and lymphatic system to another part of the body and start growing there. Once a cell has a mutation, it will pass it on every time it divides.
Oncogenes and Cancer
Mutated forms of genes involved in normal cell division are called oncogenes. They can encourage cancer growth and development.
Sometimes oncogene mutations that lead to cancer are inherited – the breast cancer genes BRCA1 and BRCA2, for instance. More commonly, mutations happen because of cancer-causing substances we’re exposed to, such as ultraviolet rays from the sun or smoking tobacco. These mutations are only found in cells that have become damaged. So, if you’re told your lung cancer has a mutation in the KRAS oncogene, this mutation is only in the lung cancer cells. You weren’t born with the mutation, it isn’t in any of the other cells of your body, and you can’t pass it on to your children.
Other Types of Cancer-Causing Gene Mutations
As well as oncogenes, there are other types of genes that contribute to cancer growth and development. One group is called tumor suppressor genes. The normal function of these genes is to stop cells from dividing when they shouldn’t. In many tumors, however, mutations in these genes mean they are lost or inactivated. This allows the cells to continue to divide and the cancer develops.
Other cancer-causing genes are called DNA repair genes. In normal cells, these genes repair damage caused to the DNA. If the DNA damage is too bad, the DNA repair gene will tell the cell to self-destruct.
Cells with mutations in these DNA repair genes are less able to repair cancer-causing mutations. They are also able to survive with DNA damage that would cause normal cells to die.
Driver Mutations
The most important gene changes in the development of cancer cells are called driver mutations – because they drive the development of a cancer. An abnormal protein produced because of a driver mutation may be key to encouraging cancer cells to keep on dividing, for example.
These important mutations are being researched as potential targets for treatment. If treatments can block the proteins that these genes make, they can help to stop cancer growth and might keep people healthy for longer.
KRAS Mutations Are Driver Mutations
Normal KRAS protein is important in the control of cell replacement and development. But KRAS mutations can produce abnormal proteins that are permanently active, instead of only working when they need to. These proteins encourage cells to multiply all the time.
There are several different mutations in the KRAS gene that we know are possible driver mutations for lung cancer. Each individual cancer is likely to have only one type of driver mutation.
Driver Mutations and Biomarkers
A biomarker is a characteristic of the body that can be measured. There are different types of biomarkers. For instance, a biomarker may be used to diagnose a disease, measure a normal body process, or show how a treatment is working.
If a diagnostic biomarker is present, that confirms a diagnosis. Some biomarkers are used to monitor a condition. For example, excess PSA is made by prostate cancer cells, so levels rise when a prostate cancer is growing.
Types of Question that Can Sometimes Be Answered by Cancer Biomarkers
- Prognostic: How aggressive is the cancer likely to be?
- Diagnostic: What type of cancer is it?
- Predictive: Is this the optimal drug for my cancer?
- Recurrence: Will the cancer return?
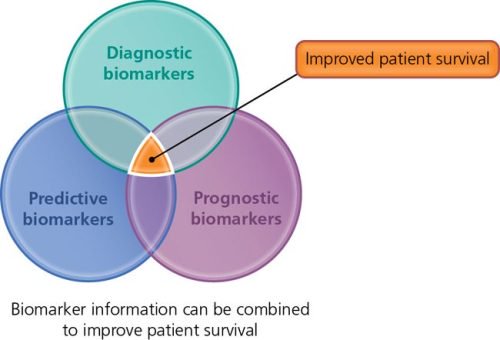
Driver mutations can also be biomarkers. If a treatment has been developed that targets a driver mutation, the presence of the abnormal protein produced as a result of the mutation in your cancer cells shows your doctor that this type of treatment could work for you. But not all cancers have a specific driver mutation.
Biomarkers in Lung Cancer
There are several different biomarkers in lung cancer. The most common include EGFR, ALK, and KRAS.
- EGFR is a gene that normally encourages cells to divide. But if mutated, it causes too much cell division, which can result in a cancer. There are several different EGFR mutations that can lead to lung cancer. Some of these can be targets for treatments called EGFR inhibitors.
- ALK is a gene that normally helps in the development of the gut and nervous system, and is switched off after this is completed in the womb. Sometimes ALK gets switched back on again, fuses with another gene, and causes lung cancer. Treatments that target ALK are called ALK inhibitors.
- KRAS is the biomarker that we’re most interested in here. You’ve been given this booklet because your lung cancer has tested positive for a specific KRAS mutation and might respond to treatment that blocks the abnormal protein made by it.
Information based on Fast Facts for Patients: Non-small Cell Lung Cancer with KRAS Mutation (Karger, 2023).





Comments
Share your opinion with us and leave a comment below!