This is the fifth part of our series about the condition based on our patient booklet “Fast Facts for Patients and Supporters: Pyruvate Kinase Deficiency”, which is freely available online. This article lists how complications can be managed when treating pyruvate kinase deficiency.
Treating Excess Bilirubin in Newborns
Most newborn babies with PK deficiency develop jaundice because of the breakdown of red blood cells and the inability of their immature livers to conjugate bilirubin.
An increase in unconjugated bilirubin in a newborn can lead to significant neurological complications, including a problem called kernicterus (damage to the brain and central nervous system). Newborns with severe jaundice therefore need treatment to decrease the bilirubin levels.
Phototherapy (light therapy) exposes your baby’s skin to as much light as possible. It lowers bilirubin levels through a process called photo-oxidation. Oxygen is added to the bilirubin, making it easier for the baby’s liver to process the bilirubin.
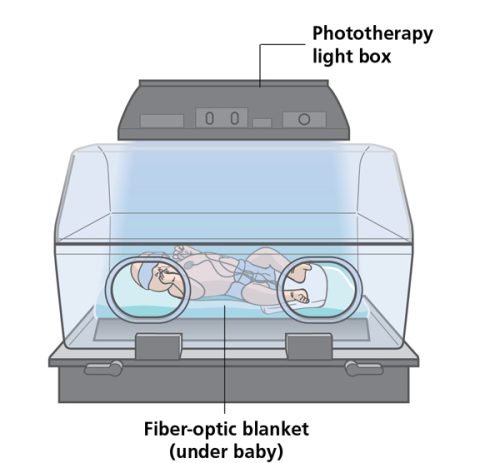
There are two main types of phototherapy:
- conventional – the baby lies under a halogen or fluorescent lamp
- fiber-optic – the baby lies on a fiber-optic blanket so that light shines on the baby’s back.
Continuous multiple phototherapy may also be offered, using more than one light and a fiber-optic blanket at the same time.
Bilirubin levels will be tested every 4–6 hours after phototherapy has started, then every 6–12 hours once the levels start to decrease.
The treatment will be stopped when the bilirubin reaches a safe level, usually within 48 hours. Intravenous fluids and/or increased feeding may also help with the clearance of the bilirubin.
Exchange transfusion. When phototherapy does not adequately decrease the bilirubin level, a procedure called exchange transfusion is recommended to avoid the risk of kernicterus.
Small amounts of your baby’s blood are removed and replaced with blood from a donor (i.e. a blood transfusion) through an intravenous catheter that is placed in their umbilical cord, arms or legs. A protein called albumin may be transfused as well to help decrease the bilirubin level.
The process can take several hours, with regular checks on bilirubin levels to make sure they are falling. If bilirubin levels remain high, the procedure may need to be repeated.
In addition to reducing the bilirubin level, this procedure raises the hemoglobin level and treats anemia.
Treatment of Iron Overload
If you receive regular blood transfusions for your PK deficiency, you will need treatment to remove excess iron from your body. If you have iron overload in the absence of transfusions, you may find you need iron removal treatment for a period of time and are then able to stop the treatment, maybe restarting it again years later based on iron monitoring results.
Depending on the degree of iron burden, drugs that remove iron from the body (chelation therapy) and/or therapeutic withdrawal of blood to remove iron from the body (phlebotomy) may be prescribed. Whether phlebotomy is an effective treatment for iron removal in PK deficiency and how it compares to iron chelation therapy have not been studied. Therefore, most patients with PK deficiency are treated with chelation for iron removal, rather than with phlebotomy.
Chelation therapy. Chelation agents bind with the iron to form substances that can be excreted from the body easily. The table overleaf provides a list of chelation medicines. Even if you receive infrequent transfusions or you’ve never received a transfusion, you may still need iron chelation treatment.
Terminology Tip: Chelation comes from the Greek word “chele”, which means “claw”, in the sense of a pincer-like claw of a lobster or crab, and suggests gripping or holding something firmly. Chelation agents bind with metals such as iron to form substances that can be easily excreted from the body.
Phlebotomy (blood draws). Phlebotomy is an alternative treatment to remove excess iron if you do not receive transfusions. A small volume of blood is removed periodically (for example, every 4 weeks) intravenously to remove the iron. The volume of blood removed will depend on your size and your baseline hemoglobin level, but may be 50–300 mL. A sample of blood will be taken before the procedure to measure your hemoglobin. Phlebotomy is safe if you have not had a transfusion and your hemoglobin is high enough to tolerate blood removal.
Gallbladder Removal (Cholecystectomy)
Gallstones can be associated with nausea or abdominal pain after eating and/or complications if they become stuck in the biliary tract.
You will have an ongoing risk of developing gallstones because of continued hemolysis. Given this, surgical removal of the gallbladder is recommended in PK deficiency if you have gallstones.

If you are considering a splenectomy, you should have an ultrasound before the procedure to see if you have gallstones. Even if you do not, you could consider having a cholecystectomy at the same time as your splenectomy, given the likelihood that you will develop gallstones in future.
Vitamin Supplements
Folic acid is needed to make red blood cells. If you have an elevated reticulocyte count, you will need to ensure you have sufficient folic acid. Depending on the amount of folic acid in your diet, you may need to take folic acid supplements.
Vitamin D/calcium. Given the risk for low bone density in people with PK deficiency, you may find it beneficial to take vitamin D and calcium supplements for bone health. This will depend on how much vitamin D and calcium you have in your diet.
Exercise can also help to strengthen your bones. If your bone density is very low, your doctor may recommend other treatments.
A note of caution: People with PK deficiency tend to overload with iron, so you must avoid taking additional iron supplements in the form of multivitamins or prenatal vitamins.
Please check out the other posts of our series here:
- What Is Pyruvate Kinase Deficiency?
- What Causes Pyruvate Kinase Deficiency and How Is It Diagnosed?
- How Will Pyruvate Kinase Deficiency Affect Me or My Child?
- Treating Pyruvate Kinase Deficiency: Managing the Anemia
Information based on Fast Facts for Patients and Supporters: Pyruvate Kinase Deficiency (Karger, 2019).





Comments
Share your opinion with us and leave a comment below!